Our targeted anti-FGFR4 monoclonal antibody therapy aims to redefine the treatment of left ventricular hypertrophy (LVH) in chronic kidney disease (CKD) - a serious complication affecting up to 80% of patients with advanced CKD. We are pioneering a novel, mechanism-based therapeutic strategy in an area with very limited treatment options
More than 850 million people worldwide are living with CKD
The IMPACT CKD model projects a 7.7% increase in the global CKD population by 2032
Over 90% of patients with CKD develop left ventricular hypertrophy (LVH)
Cardiovascular disease is the leading cause of mortality in CKD at every disease stage
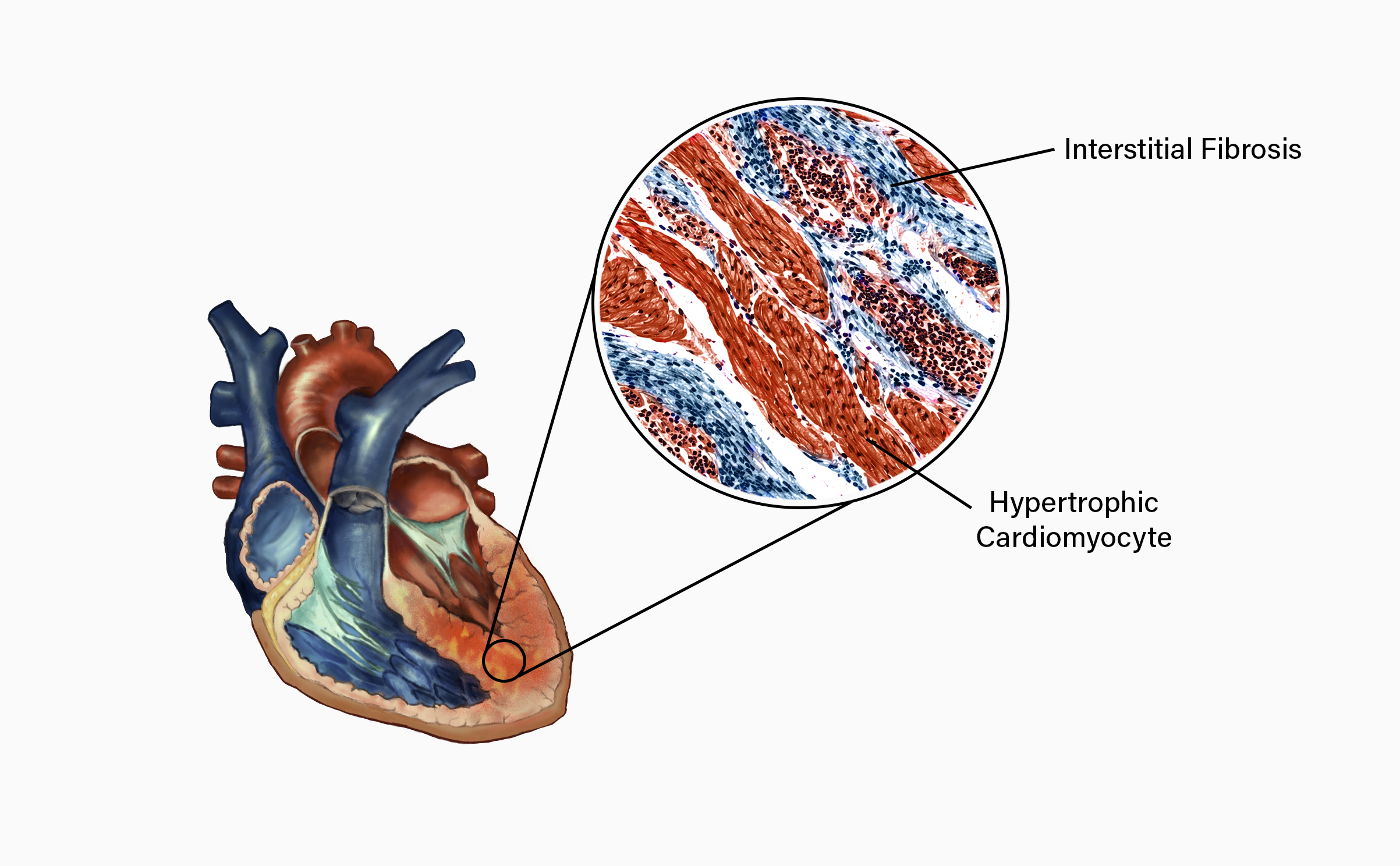
In chronic kidney disease (CKD), circulating levels of fibroblast growth factor 23 (FGF23) are markedly elevated and are strongly linked to left ventricular hypertrophy (LVH) and an increased risk of cardiovascular disease. CKD leads to excessive and sustained FGF23 production, which can inappropriately activate fibroblast growth factor receptor 4 (FGFR4) on cardiomyocytes. This aberrant FGF23–FGFR4 signaling promotes pathological cardiac remodeling, resulting in cardiomyocyte hypertrophy and myocardial fibrosis. These structural changes compromise both cardiac relaxation (diastolic function) and contraction (systolic function), contributing significantly to the excessive cardiovascular morbidity and mortality observed in patients with CKD.
Our highly selective monoclonal antibody specifically inhibits FGF23-driven activation of fibroblast growth factor receptor 4 (FGFR4), thereby blocking the initiation of maladaptive, pro-hypertrophic signaling pathways in cardiomyocytes. By selectively targeting FGFR4, the antibody can disrupt the pathological FGF23-FGFR4 signaling axis while preserving other physiological functions of FGF23. This targeted inhibition can potentially maintain normal intracellular signaling, prevent maladaptive cardiac hypertrophy and fibrosis, and support the preservation of normal cardiac structure and function, even under conditions of chronically elevated FGF23.